A New Technique for Successful Management of a Complete Suprahepatic Caval Transection
Ignazio R Marino, MD, FACS, Fabrizio di Francesco, MD, Cataldo Doria, MD, Salvatore Gruttadauria, MD,
Augusto Lauro, MD, Victor L Scott, MD
PATIENT AND TECHNIQUE
In June 2001, a 17-year-old girl was involved in a high-speed motorcycle crash. She was taken to a local hospital, where multiple large, actively bleeding lacerations of the spleen and right lobe of the liver were found. A splenectomy was performed and a profuse hemorrhage from the right lobe of the liver was detected. Silk stitches were placed between the liver and the diaphragm to provide a tamponade effect. Possibly, the sutures created a watertight compartmentable to tamponade the bleeding and to support the systemic venous return and filling pressure.Hemostasiswas unsuccessful and, at this time, no vena caval injury was suspected. After packing, the abdomen was closed and the patient was transported, intubated and ventilated, to our institution by helicopter. The patient had mydriasis and was hypothermic with a temperature of 34.5°C and pH of7.13. Rapid fluid volume resuscitation was performed and the patient was taken to the operating room. Hemoperitoneumof > 5 L was present, and extensive bleeding was noted to be originating from a deep laceration of the VII and VIII hepatic segments. After removing the packing and sutures between the liver parenchyma and diaphragm, the retrohepatic segment of the IVC was exposed. When mobilization of the right lobe was attempted, blood pressure dropped to a critical level. For this reason, a large injury of the suprahepatic IVC was strongly suspected. It was then decided to attempt a direct approach to the juxtadiaphragmatic segment of the IVC by putting the patient on atrialcavalvenous-venous bypass (VVB), which was achieved by performing a sternotomy to gain control of the extrapericardial segment of the IVC and right atrium. At that point,a left saphenofemoral cutdown was obtained to initiateatrial-caval VVB and to perform direct repair of the suspected IVC transection. A purse-string suture in the right atrial appendage was placed and the intrapericardial IVC was snared by umbilical tape. A 26F catheter was placed inside the right atrium. A 20F venous catheter was placed in the IVC through the left femoral and iliac vein and the VVB was initiated using a centrifugal pump. Simultaneously with starting of the VVB, a Pringle maneuver was performed with the snaring of umbilical tape (Fig. 1A).Cannula tubing and connectors were heparin-bonded; no other heparin was used during the operation. The diaphragm was divided in its midportion directly anterior to the IVC. Atthat point, the right lobe of the liver was entirely mobilized,exposing the retrohepatic IVC. The juxtadiaphragmatic IVC was, in fact, completely transected and the right supra hepaticve in was disconnected from the IVC.Two 3-0 polypropylene sutures were placed as right and left corner sutures to expose the transected edges of the IVC. Suprahepatic IVC reconstruction was performed by end to end anastomosis with 3-0 polypropylene running suture, using the same technique as in orthotopic liver transplantation. At the end of this anastomosis,the transected right suprahepatic vein was treated by suturing the proximal and distal stumps by polypropylene 5-0stitches (Fig. 1B). The liver was then reperfused by first releasing the Pringle maneuver, then by opening the clamp, occluding the suprarenal IVC and, finally, by releasing the tourniquet binding the intrapericardial IVC. Total time of the Pringle maneuver was 36 minutes. Total atrial-caval VVB time was 40 minutes. At that point, segments VII and VIII were substantially devitalized and a wedge resection was carried out.
Compressive packing of the liver was performed after irrigation with warm saline and antibiotics.Successful hemostasis was finally achieved. Sternotomy and the abdominal wall were closed and the skin was left open.
During the operation, 26 U packed red blood cells and 18 U fresh-frozen plasma were transfused. The patient was taken to the intensive care unit in hemodynamically stable condition. Six hours after the operation,the patient, remaining hemodynamically stable with an adequate urine output, had awakened and started moving her arms. The fixed mydriasis was resolved.
 Figure 1. (A) An atrial-caval venous-venous bypass (1) with a centrifugal pump (Bio-Medicus) was used to achieve total hepatic vascular exclusion. Application of this device was associated with cross-clamping of the suprarenal inferior vena cava (2) and a standard Pringle maneuver (3). Intrapericardial inferior vena cava was also clamped with a tourniquet (4). (B) Reconstruction of the vena cava was obtained by end to end anastomosis of the suprahepatic inferior vena cava (1). Proximal (2) and distal (3) stumps of the right hepatic vein were sutured. Segments VII and VIII were suffering for outflow obstruction and seemed devitalized. A wedge resection was performed. (Reprinted with permission of the artist, Jon Coulter.)
Figure 1. (A) An atrial-caval venous-venous bypass (1) with a centrifugal pump (Bio-Medicus) was used to achieve total hepatic vascular exclusion. Application of this device was associated with cross-clamping of the suprarenal inferior vena cava (2) and a standard Pringle maneuver (3). Intrapericardial inferior vena cava was also clamped with a tourniquet (4). (B) Reconstruction of the vena cava was obtained by end to end anastomosis of the suprahepatic inferior vena cava (1). Proximal (2) and distal (3) stumps of the right hepatic vein were sutured. Segments VII and VIII were suffering for outflow obstruction and seemed devitalized. A wedge resection was performed. (Reprinted with permission of the artist, Jon Coulter.)
On postoperative day 5, the patient returned to the operating room to have the hepatic packing removed and to achieve complete hemostasis. The liver was still congested and edematous, and there was some oozing from the remnant of segments VII and VIII. After 24hours, the patient was extubated and transferred to the floor. On postoperative day 25, angiogram of the IVC demonstrated no leak and no vena caval stenosis (Fig. 2).On postoperative day 28, the patient was discharged with normal laboratory results. Six years after the operation,the patient is in very good health with normal liver function and is currently attending law school.
DISCUSSION
The exceedingly high mortality of suprahepatic IVC trauma indicates the need for standardization of the surgical technique in patients with this kind of caval injury.
It has long been recognized that abdominal vascular injuries sustained by trauma patients are highly lethal.Among these injuries, those to the IVC, particularly in the retrohepatic portion, and major hepatic veins, are the most fatal.1-16 The high lethality from IVC injuries has been attributed to its surgically inaccessible location and to the difficulty exposing and controlling the hemorrhage.10,11
Injury location is the most important determinant of mortality, with a reported rate of 100% when the lesion is a transection of the suprahepatic segment of the IVC.1-4,7,8,10,11,17,18
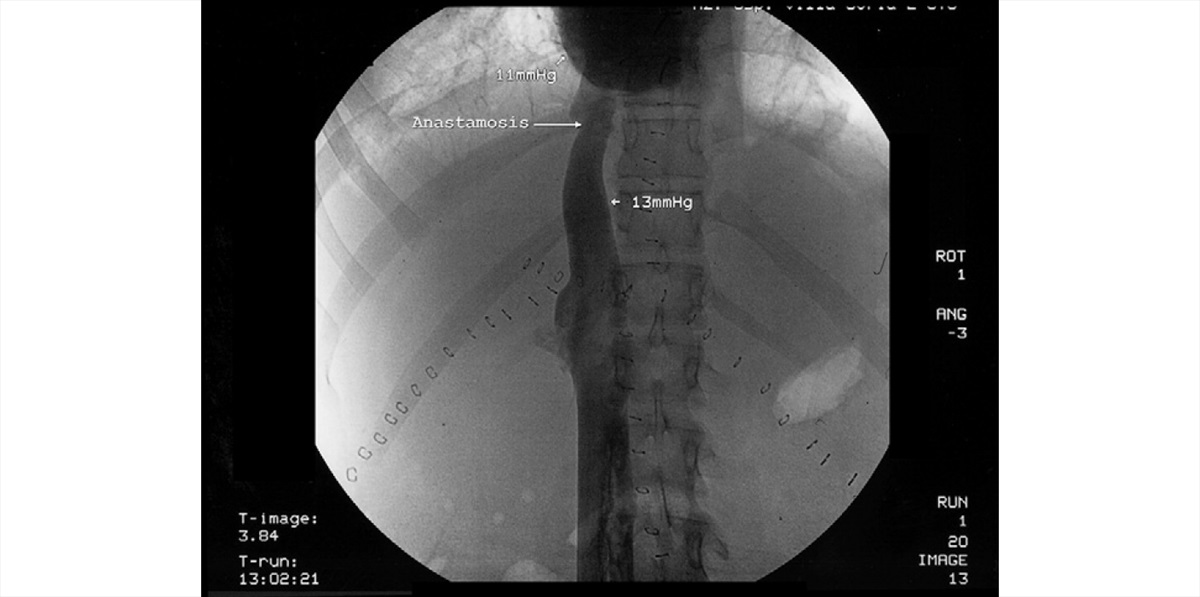
Figure 2. Angiogram of the inferior vena cava on postoperative day 25, showing no caval strictures.
Often, as in the patient reported here, a key role is played by the presence of a retroperitoneal hematoma. Detection and clinical importance of the retroperitoneal hematoma in penetrating wounds of the IVC were first reported in 1957 by Starzl and colleagues.19
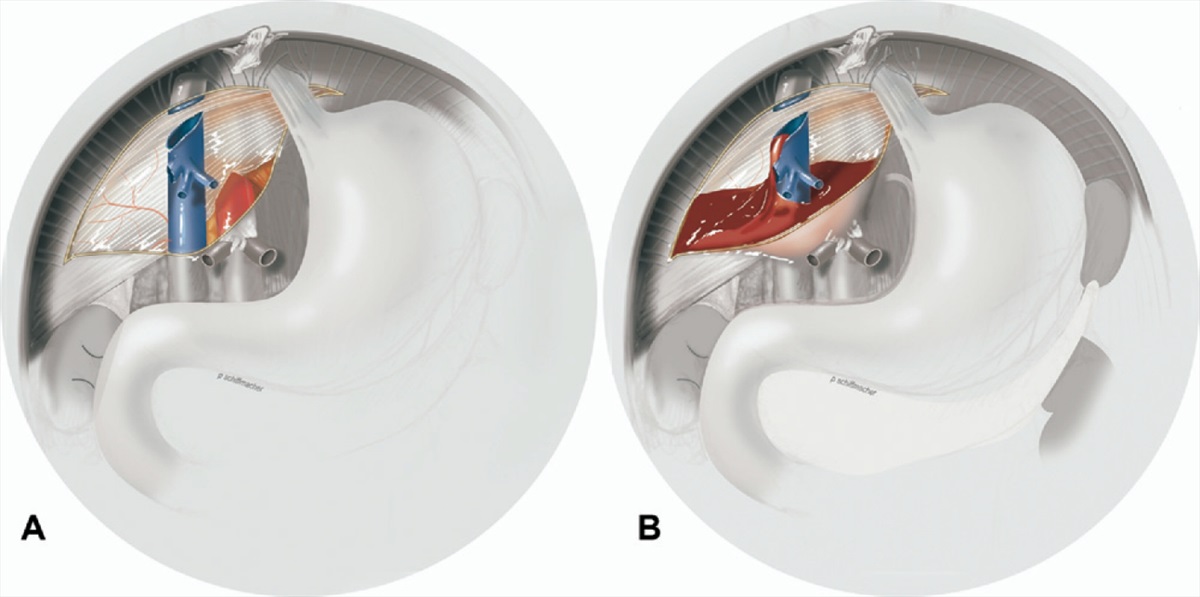
Figure 3. (A) Bare area and injury pattern. Peritoneal reflections of the liver leave a bare area at the posteromedial surface of the right lobe between the superior and inferior layers of the coronary ligament.
The cava is completely transected by the trauma. (B) The bare area contained the blood from the transection of the suprahepatic inferior vena cava by creating a retroperitoneal hematoma.
It was already emphasized then that active bleeding can cease by the time of laparotomy because of a hematoma surrounding the caval injury and that serious bleeding does not occur until the retroperitoneal space is entered.19-21
A vena cava injury should always be suspected if a retroperitoneal hematoma is present. Exploring the hematoma blindly is the crucial mistake that should be avoided. As a clinical demonstration of this concept, several reports have described the massive fatal hemorrhage after decompression of a hematoma coveringan IVC injury.6,19-23 The integrity of the natural structures capable of containing the blood and of tamponading the bleeding around the liver has a remarkable clinical importance. The peritoneal reflections of the liver leave a bare area at the posteromedial surface of the right lobe between the superior and inferior layers of the coronary ligament; this area is extraperitoneal. Because the retrohepatic IVC occupies the left or media llimit of the bare area, any bleeding caused by a retrohepatic IVC trauma is temporarily contained by the ligamentous structures delimiting this bare area. IP bleeding might not immediately occur or can be delayed. The sequence of events presented in this article should serve as an indication to a new strategic approach to this criticalc ondition. Fortunately, in our patient, the retroperitoneal hematoma had not been entered during the firs tlaparotomy performed on the patient at the previous hospital (Fig. 3). These patients warrant a standby VVB.In fact, the other key point in management of our patient was the choice of a direct approach by putting the patient in atrial-caval VVB to work in a bloodless field through complete hepatic vascular exclusion. Liver vascular exclusion requires control of the suprahepatic andi nfrahepatic IVC, the hepatic artery, and the portal vein.Clamping of the IVC in a hypovolemic patient can lead to cardiac arrest because of the sudden decrease in cardiac preload.23-25
At the time of abdominal exploration,when Pringle maneuver fails to control the hemorrhage or when there is continuous bleeding from behind the right lobe, a suprahepatic IVC injury should always be suspected.13
In our patient, presence of the retroperitoneal hematoma and the critical decrease of blood pressure at every attempt to mobilize the liver prompted us to implement a new surgical approach. The hepatic packing and manual compression offered sufficient time to establish an atrial-caval VVB. The VVB provided us the opportunity to work in a bloodless field and safely perform the vascular repairs without compromising venous return. Blunt injuries can also lead to avulsion of the hepatic veins from the IVC in combination with lacerations of the liver surface. Buckman and colleagues23 described two general juxtahepatic venousinjury-wounding patterns: one (type A) in which the venous injury is intraparenchymal, with bleeding predominantly through the disrupted liver; and the other(type B), in which the venous lesion is extraparenchymal,with bleeding predominantly around the liver. Our patient presented us with a situation similar to the type B wounding pattern with a rupture of the VII and VIII hepatic segments, avulsion of the right hepatic vein, and, mainly, complete transection of the suprahepatic IVC. A concomitant parenchymal hepatic injury is a major aggravating risk factor because of the greater difficulty in achieving a bloodless field and the considerable expertise required for carrying out the necessary surgical repair. For injuries of the suprahepatic IVC segment between the right atrium and the take-off of the hepatic veins, 100% mortality is reported.1-4,7,8,10,11,17,18
The major cause of death is the uncontrollable bleeding,which occurs during the attempt to expose and repair the suprahepatic IVC. This leads to exsanguination and intraoperative death. Any attempt to rotate the liver to achieve better exposure of the IVC increases the blood loss and gives rise to additional risks of air embolism. For these reasons, when bleeding control is not achievable and substantial expertise and technical support are nota vailable, the swift transfer of the patient, after intraabdominal packing of the liver, to a facility where liver operations and liver transplantation are routinely performed,can be a life-saving strategy. Simple vascular clamping, atriocaval surgical shunting, hepatic resection,and perihepatic packing have been the methods oftreatment reported in the literature. Attempts to successfully manage a suprahepatic IVC transection have been reported with negative results.1-4,7,8,10,11,17,18
Standardization of a surgical approach for this kind of rare but lethal condition has yet to be successfully achieved.It is imperative to obtain control of the bleeding and maintain a bloodless surgical field through a short liver ischemia time (fewer than 50 minutes), while the patient is kept hemodynamically stable.We strongly believe that use of a modified atrial-caval VVB played a key role in successfully managing this kind of IVC lesion. We are now convinced that this is the only safe and possible way to achieve anatomic control of the suprahepatic IVC to perform a direct repair. An alternative technique, still borrowing from live rtransplantation experience, could have avoided sternotomya nd atrial bypass and favored instead the classic VVB often used during liver transplantation, performed from the femoral vein into the axillary vein after cutdown,or into one of the ports of a central line placed inthe neck. Adopting such a method, a clamp could be placed on the suprahepatic IVC at the cavoatrial junction after opening the pericardium vertically and entering the pericardial cavity from the abdomen, allowing good visualization of the cavoatrial junction. This can prevent possible morbidity related to a sternotomy. Because of the critical emergency situation and the uncertainties of the anatomy of the lesion, we opted for more direct access to the cavoatrial junction.In similar extreme cases, the first goal is to achieve bleeding control through total vascular occlusion beforere pairing the injury. To the best of our knowledge, this is the first description of successful management of a complete traumatic transection of the suprahepatic IVC.With this article, we would like to introduce a new technique of atrial-caval VVB, which is a ripple extension of the basic technique of liver transplantation. Any retroperitoneal hematoma should not be entered until total vascular exclusion through atrial-caval VVB has been established. Based on our experience and a thorough review of the literature, this approach would seem to be the safest and most successful one to pursue.
REFERENCES
1.Wiencek RG,Wilson RF. Abdominal venous injuries. J Trauma1986;26:771–778.
2. Klein SR, Baumgartner FJ, Bongard FS. Contemporary management strategy for major inferior vena caval injuries. JTrauma1994;37:35–41.
3. Asensio JA, Chahwan S, Hanpeter D, et al. Operative management and outcome of 302 abdominal vascular injuries. Am JSurg 2000;180:528–533.
4. Khoury G, Sfeir R, Khalifeh M, et al. Penetrating trauma to the abdominal vessels. Cardiovasc Surg 1996;4:405–407.
5. Jan WA, Samad A, Anwar R. Mortality and morbidity of abdominal inferior vena-caval injuries. J Coll Physicians Surg Pak2004;14:622–625.
6. Ochsner JL, Crawford ES, De Bakey ME. Injuries of the vena cava caused by external trauma. Surgery 1961;49:397–405.
7. Burch JM, Feliciano DV, Mattox KL, et al. Injuries of the inferiorv ena cava. Am J Surg 1988;156:548–552.
8. Graham JM,Mattox KL, Beall AC Jr, et al.Traumatic injuries of the inferior vena cava. Arch Surg 1978;113:413–418.
9. Burns GR, Sherman RT. Trauma of the abdominal aorta and inferior vena cava. Am Surg 1972;38:303–306.
10. Weichert RF 3rd, Hewitt RL. Injuries to the inferior vena cava:report of 35 cases. J Trauma 1970;10:649–657.
11. Turpin I, State D, Schwartz A. Injuries to the inferior vena cava and their management. Am J Surg 1977;134:25–32.
12. Burch JM, FelicianoDV,Mattox KL.The atriocaval shunt. Facts and fiction. Ann Surg 1988;207:555–568.
13. Chen RJ, Fang JF, Lin BC, et al. Surgical management of juxtahepaticvenous injuries in blunt hepatic trauma. JTrauma 1995;38:886–890.
14. Quast DC, Shirkey AL, Fitzgerald JB, et al. Surgical correction of injuries of the vena cava: an analysis of sixty-one cases.J Trauma 1965;147:3–10.
15. Yellin AE, Chaffee CB, Donovan AJ. Vascular isolation in treatmentof juxtahepatic venous injuries. Arch Surg 1971;102:566–573.
16. Kudsk KA, Sheldon GF, Lim RC Jr. Atrial-caval shunting (ACS)after trauma. J Trauma 1982;22:81–85.
17. CogbillTH,Moore EE, Jurkovich GJ, et al. Severe hepatic trauma:a multi-center experience with 1,335 liver injuries. JTrauma 1988;28:1433–1438.
18. Buechter KJ, Sereda D, Gomez G, et al. Retrohepatic vein injuries:experience with 20 cases. J Trauma 1989;29:1698–1704.
19. Starzl TE, Broadway RK, Dever RC, et al. The management of penetrating wounds of the inferior vena cava. Ann Surg 1957;23:455–461.
20. Starzl TE, Kaupp HA Jr, Beheler EM, et al. Penetrating injuries of the inferior vena cava. Surg Clin North Am 1963;43:387–400.
21. Starzl TE, Kaupp HA Jr, Beheler EM, et al. The treatment of penetrating wounds of the inferior vena cava. Surgery 1962;51:195–204.
22. Buckman RF, Pathak AS, Badellino MM, et al. Injuries of the inferior vena cava. Surg Clin North Am 2001;81:1431–1447.
23. Buckman RF Jr, Miraliakbari R, Badellino MM. Juxtahepaticvenous injuries: a critical review of reported management strategies.J Trauma 2000;48:978–984.
24. Biffl WL, Moore EE, Franciose RJ. Venovenous bypass and hepatic vascular isolation as adjuncts in the repair of destructive wounds to the retrohepatic inferior vena cava. J Trauma 1998;45:400–403.
25. Baumgartner F, ScudamoreC,Nair C, et al.Venovenous bypass formajor hepatic and caval trauma. J Trauma 1995;39:671–673.
 06.60301809
06.60301809