Sheep in Wolf’s Clothing: Pedunculated Colonic Lipoma with Overlying Hyperplastic and Ulcerated Epithelium
Rossella Palma · Stefano Pontone · Ignazio Roberto Marino · Fabio Massimo Magliocca · Stefano Frattaroli ·Valeria Tonini · Vito D’Andrea
Published online: 10 March 2020
© Springer Science+Business Media, LLC, part of Springer Nature 2020
Abstract
Introduction Lipomas are the most common non-epithelial benign tumors of the gastrointestinal tract with a reported incidence in the colon of 0.2–4.4%. These lesions are usually asymptomatic with a typical endoscopic finding of a smooth, slightly yellow, circular, polyp that is sessile in most cases, covered with normal colonic mucosa.
Areas Covered There are rare reported cases of alterations of the overlying mucosa such as hyperplasia, atrophy, adenomatous changes, and necrosis.
Expert Commentary We report a rare case of pedunculated colonic lipoma of the transverse colon covered with hyperplastic and ulcerated epithelium easily misdiagnosed as an adenomatous lesion.
Abbreviations
EMR Endoscopic mucosal resection
FOBT Fecal occult blood test
Introduction
Lipomas are the most common non-epithelial benign tumors of the gastrointestinal tract with a reported incidence of 0.2–4.4% [1]. The reported prevalence is higher in women and in patients 50–60 years old, distributed in the ascending (45%), sigmoid (30.3%), descending (15.2%), and transverse colon (9.1%). These lesions are usually asymptomatic with a typical endoscopic finding of a smooth, slightly yellow, circular polyp, sessile in the most of cases, with a normal colonic superficial mucosa [2]. Nevertheless, in about 25% of cases, and especially when their maximum diameter is > 2 cm, clinical symptoms such as iron deficiency anemia, abdominal pain, constipation, bleeding, and intussusception may occur. There are rare reported cases of alterations of the overlying mucosa such as hyperplasia, atrophy, adenomatous changes, and necrosis [3–7].
Herein we report a case of colonic lipoma covered with hyperplastic and ulcerated epithelium that was easily confused with an adenoma.
Case Report
A 74-year-old woman underwent routine screening colonoscopy for positive FOBT detection. She denied constipation, diarrhea, hematochezia, or other gastrointestinal symptoms. Her past medical history and biochemical examinations were unremarkable.
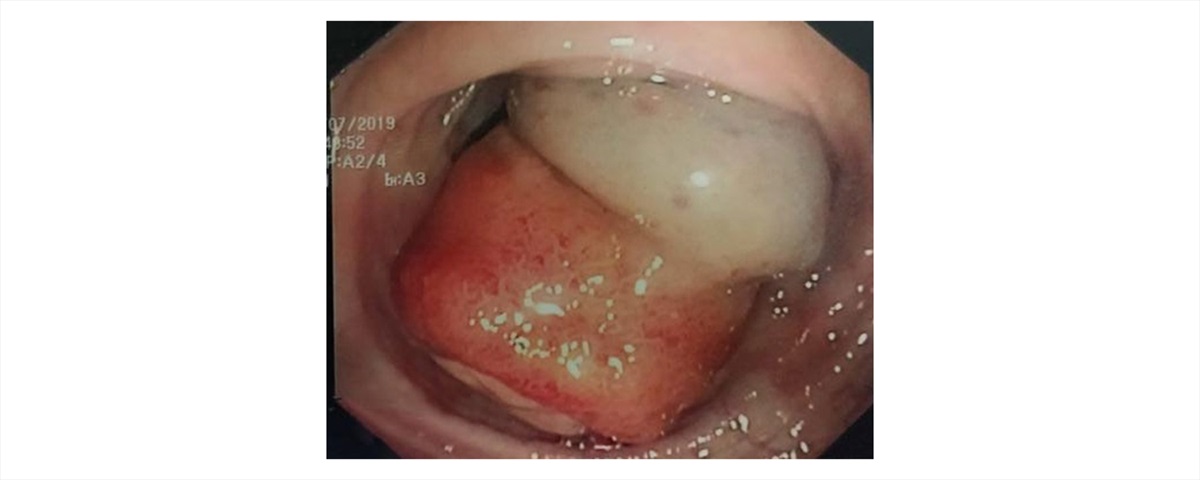
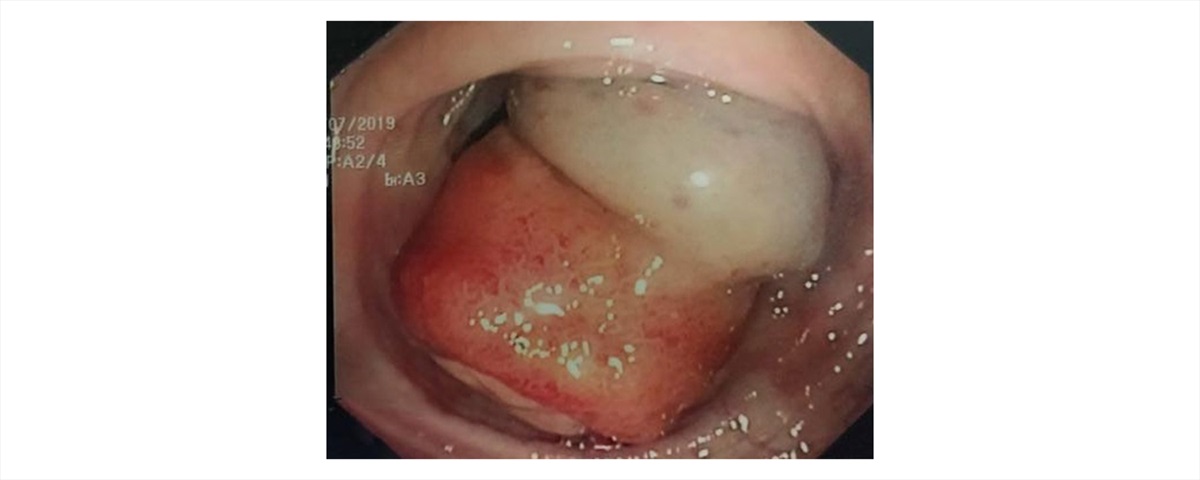
Fig. 1 Endoscopic finding of a pedunculated polyp with ulcerated and slightly irregular superficial epithelium
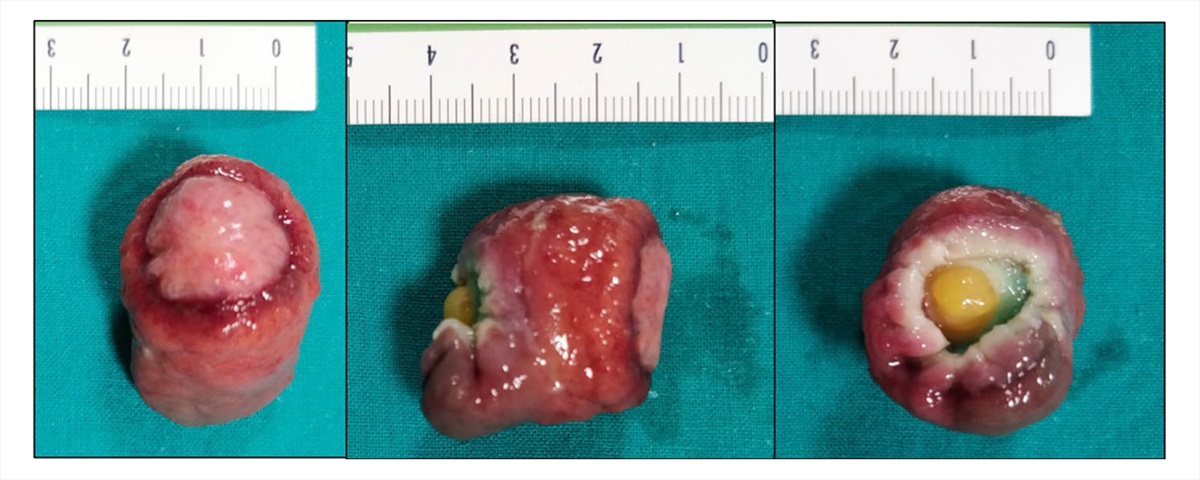
During colonoscopy, a 30-mm pedunculated polyp in the transverse colon was identified. The superficial epithelium was macroscopically ulcerated, friable, and slightly irregular (Fig. 1). The polyp did not display the characteristic features of a lipoma (such as the “pillow sign”) but more resembled an epithelial lesion. We performed an EMR after submucosal saline solution injection (Fig. 2). Histopathological examination showed a benign tumor arising from the submucosal layer, composed of mature adipose tissue covered by superficially ulcerated hyperplastic epithelium (Fig. 3). The lesion was completely resected.
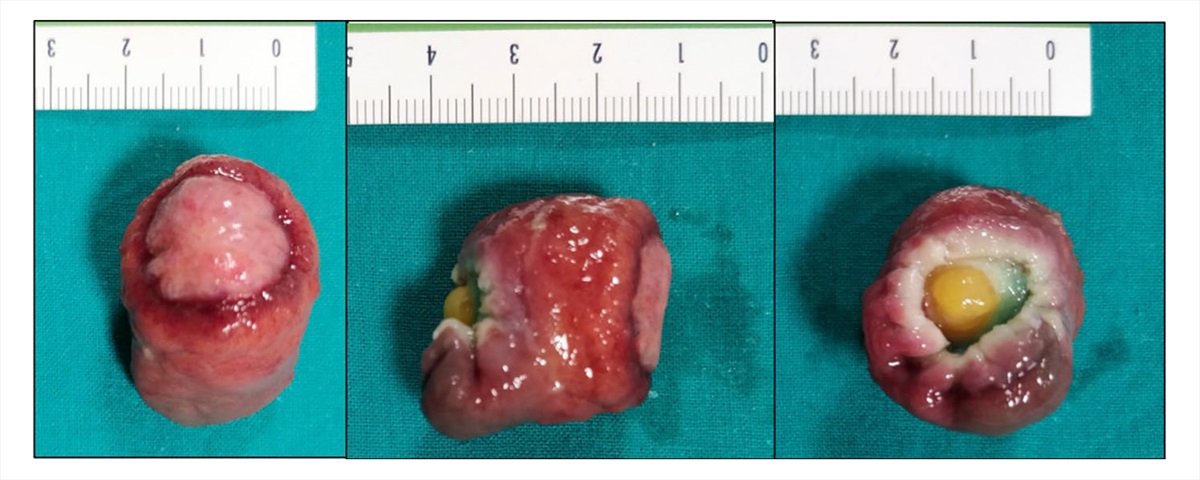
Fig. 2 Endoscopic Mucosal Resection (EMR): macroscopic aspect
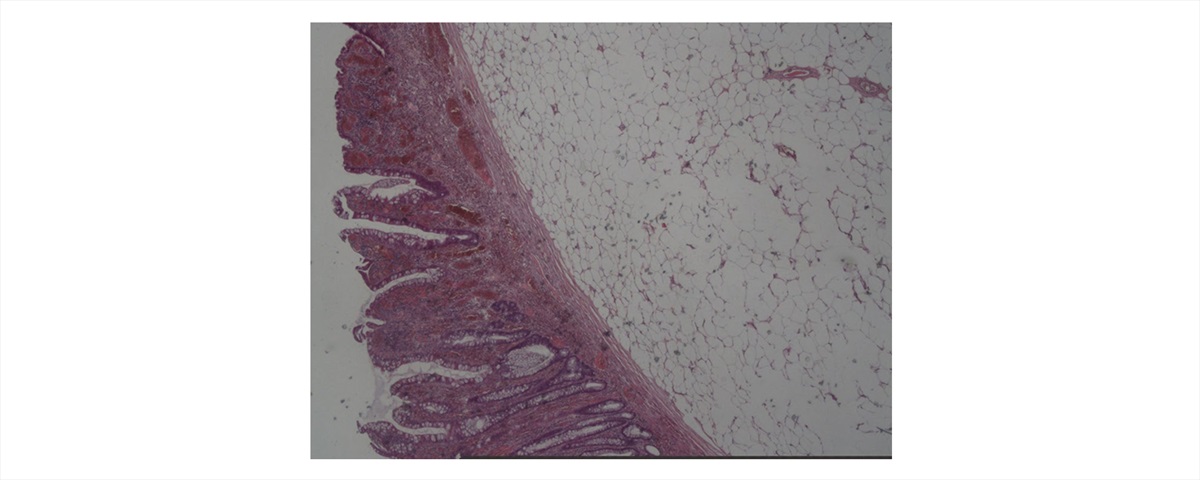
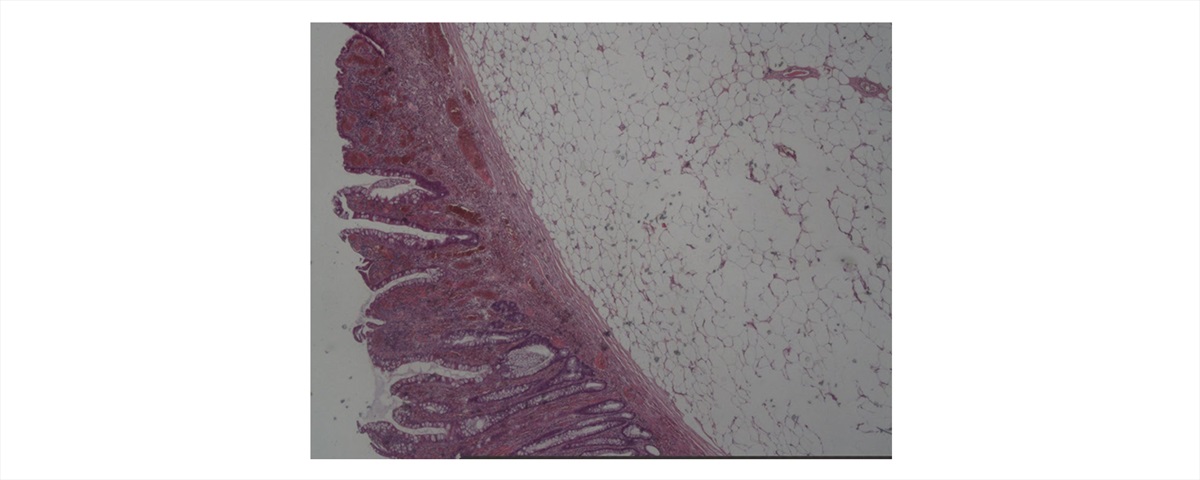
Fig. 3 Microscopic examination showing a colonic lipoma with overlying hyperplastic epithelium
Discussion
Colonic lipomas are benign tumors amply described in the literature. These benign tumors arise from the submucosal layer and in about 10% of cases from the subserosal or intermucosal layer. The usual endoscopic appearance is a smooth, slightly yellow, rounded polyp with a thick stalk or broad-based attachment [2]. Characteristic endoscopic features include the “tenting sign” (when grasping the overlying mucosa), the “pillow sign” (pressing forceps against the lesion results in depression or pillowing of the mass), and the “naked fat sign” (extrusion of yellowish fat after biopsy) [1, 2]. Pathological examination usually shows wellcircumscribed, mature adipose tissue with varying amounts of fibrous stroma covered with intact colonic mucosa.
Categorizing the pathological features of colonic lipomas can be challenging, in particular since their oncological significance is poorly defined [8]. Snover [9] introduced the term “atypical” to indicate lipomas exhibiting cytological alterations in the fat cells (hyperchromasia, pleomorphism, and mitosis), suggestive of sarcomatous changes. Currently, the term could be extended to all lesions with hyperplastic or adenomatous changes of the overlying epithelium, as previously described by Virgilio et al. [8]. They also proposed a classification of “atypical” lipoma in type A, type B, and type C based on the malignant alterations of the covering epithelium, reporting very few cases from the literature. Although the etiology of alterations of the colonic mucosa is unknown, chronic trauma due to the passage of stools may lead to hyperplasia and adenomatous transformation of the overlying mucosa in addition to ischemic and inflammatory
mechanisms [8].
To the best of our knowledge, hyperplastic changes on the surface of a colonic lipoma have been previously reported twice. Radhi et al. [3] reported the case of a large lipoma of the sigmoid colon that was detected during a surgical intervention in a patient with diverticulitis, and Yeom et al. [5] described the case of an EMR performed on a 9-mm colonic lipoma with overlying hyperplastic epithelium located in the ascending colon.
In conclusion, we report a case of a rare pedunculated colonic lipoma, located in the transverse colon, with overlying hyperplastic and ulcerated epithelium. Even though consensus exists such that small (< 2 cm) asymptomatic colonic lipomas do not need any intervention, in our opinion the endoscopic prophylactic removal of these lesions should be considered, paying attention to the overlying mucosal changes, due to their potential for malignant transformation [4, 6–9].
References
1. Vecchio R, Ferrara M, Mosca F, et al. Lipomas of the large bowel. Eur J Surg. 1996;162:915–919.
2. Bardají M, Roset F, Camps R, et al. Symptomatic colonic lipoma: differential diagnosis of large bowel tumors. Int J Colorectal Dis. 1998;13:1–2.
3. Radhi JM, Haig TH. Lipoma of the colon with overlying hyperplastic epithelium. Can J Gastroenterol. 1997;11:694–695.
4. Seong Jun C, Joon Sung K, Byung WK. Tubular adenoma overlying a colonic lipoma resected by endoscopic resection with use of a detachable endoloop. Gastrointest Endosc. 2019;89:4.
5. Yeom J-O, Kim S-Y, Jang E-C, et al. Colonic lipoma covered by hyperplastic epithelium: case report. World J Clin Cases. 2013;1:124–127.
6. Moschetta M, Virelli R, Laricchia F, et al. Lipoma of the transverse colon covered by Tubulovillous adenoma: a rare indication for surgical treatment. Chir Gastroenterol. 2018;39:63–66.
7. Capra F, Zorcolo L, Scintu F, et al. Giant sigmoid lipoma covered by a villous adenoma. Int J Colorectal Dis. 2007;22:563–564.
8. Virgilio E, Mercantini P, Cavallini M. Is endoscopic resection a correct treatment for atypical gastrointestinal lipomas? World J Clin Cases. 2016;4:30–32.
9. Snover DC. Atypical lipomas of the colon. Report of two cases with pseudomalignant features. Dis Colon Rectum. 1984;27:485–488.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
 06.60301809
06.60301809